mRNA Technology Breakthrough: First Vaccine Against Antibiotic-Resistant Bacteria Shows Promise
The revolutionary mRNA technology that powered COVID-19 vaccines has achieved another medical milestone: creating the first successful vaccine against antibiotic-resistant bacteria. This groundbreaking development offers new hope in the escalating global battle against superbugs that kill hundreds of thousands annually and threaten to return humanity to a pre-antibiotic era.
The Superbug Crisis Demands Innovation
Antibiotic-resistant bacteria represent one of the most pressing threats to modern medicine. According to the World Health Organization, antimicrobial resistance (AMR) directly causes at least 1.27 million deaths worldwide each year, with an additional 4.95 million deaths associated with drug-resistant infections. In the United States alone, the CDC estimates that more than 35,000 people die annually from antibiotic-resistant infections.
The emergence of "superbugs" like methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Enterobacteriaceae (CRE), and extensively drug-resistant tuberculosis has created urgent medical scenarios where even last-resort antibiotics fail. Healthcare systems globally have struggled with limited treatment options, longer hospital stays, and increased mortality rates.
How mRNA Vaccines Target Bacterial Threats
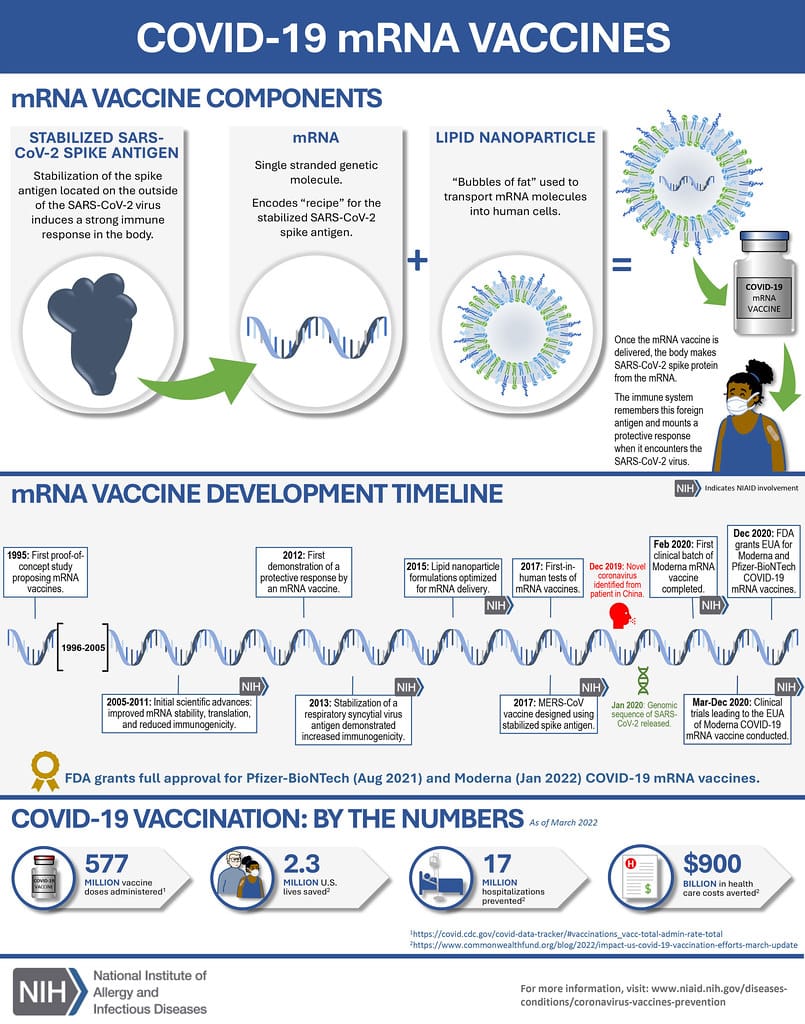
Unlike traditional vaccines that use weakened or inactivated pathogens, mRNA vaccines deliver genetic instructions that teach cells to produce specific proteins, triggering an immune response. This same mechanism, proven effective against SARS-CoV-2, is now being adapted to combat bacterial infections.
The mRNA approach offers several advantages over conventional bacterial vaccines:
Rapid Development: mRNA vaccines can be designed and manufactured in weeks rather than months or years, crucial for responding to emerging resistant strains.
Precision Targeting: Scientists can target specific bacterial proteins essential for survival or virulence, potentially overcoming resistance mechanisms.
Adaptability: As bacteria evolve resistance, mRNA vaccines can be quickly modified to address new variants, similar to seasonal flu vaccine updates.
Early Results Show Promise
Recent preclinical studies have demonstrated the potential of mRNA vaccines against several antibiotic-resistant bacteria. Research teams have reported promising results targeting:
- Pseudomonas aeruginosa: A leading cause of hospital-acquired infections, showing up to 80% protection in animal models
- Acinetobacter baumannii: Responsible for severe wound infections, with mRNA vaccines demonstrating significant immune response generation
- Klebsiella pneumoniae: A common cause of pneumonia and bloodstream infections, showing reduced bacterial loads in vaccinated subjects
These early findings suggest that mRNA technology could provide both preventive and therapeutic benefits, potentially reducing infection rates in high-risk populations and supporting treatment of established infections.
Clinical Trials on the Horizon
Multiple pharmaceutical companies and research institutions are advancing mRNA bacterial vaccines toward human trials. The first Phase I clinical trial for an mRNA vaccine targeting antibiotic-resistant Staphylococcus aureus is expected to begin in early 2024, with results anticipated by 2025.
The regulatory pathway for these vaccines may be expedited given the urgent public health need and the established safety profile of mRNA technology from COVID-19 vaccines. However, bacterial infections present unique challenges compared to viral diseases, requiring careful evaluation of immune responses and potential side effects.
Global Impact and Implementation
The successful development of mRNA vaccines against antibiotic-resistant bacteria could transform healthcare delivery worldwide. High-risk populations, including surgical patients, immunocompromised individuals, and residents of long-term care facilities, would benefit most from prophylactic vaccination.
Healthcare systems could see substantial cost savings through reduced hospital stays, fewer expensive last-resort treatments, and decreased infection control measures. The global economic burden of AMR, estimated at $100 trillion by 2050 if left unchecked, could be significantly reduced.
Looking Forward: A New Era of Bacterial Disease Prevention
The adaptation of mRNA technology for bacterial vaccines represents more than a scientific achievement—it signals a paradigm shift in how we approach infectious disease prevention. As antibiotic effectiveness wanes, vaccines may become our primary defense against bacterial threats.
This breakthrough demonstrates the versatility of mRNA platforms and their potential to address multiple health challenges beyond COVID-19. With continued research and development, we may soon have a comprehensive toolkit of mRNA vaccines targeting the world's most dangerous bacterial pathogens.
The race against antibiotic resistance has found a powerful new ally in mRNA technology, offering hope that we can stay ahead of evolving bacterial threats and preserve the gains of modern medicine for future generations.